Putting more people in jail linked to more deaths outside prison walls
Jails make areas around them sicker. (AP Photo/Eric Gay)
Negative effects of jail extend beyond the correctional facility's walls, according to a new study by U.S. researchers, who found that increases in the incarceration rate were associated with statistically significant upticks in death due to infectious diseases, substance abuse, suicide and other factors in surrounding areas.
Specifically, the researchers said in a Lancet Public Health paper published Tuesday that the addition of one prisoner per 1,000 residents of a given county is associated with a 6.5% increase in deaths from infectious disease, a 4.9% increase in deaths due to respiratory disease, a 2.6% increase in substance abuse-related deaths and a 2.5% increase in suicides within that county after one year. The deaths examined were among individuals under 75 years old.
"Jails are an important driver of infectious disease spread and death across entire counties," said lead author Sandhya Kajeepeta, a doctoral epidemiology student at Columbia University, in an interview. "We're seeing a growing body of evidence that jails are threatening our safety rather than keeping us safe."
Kajeepeta and her co-authors also found smaller associations between increases in inmate populations and deaths due to heart disease, cancer, stroke, diabetes and unintentional injuries.
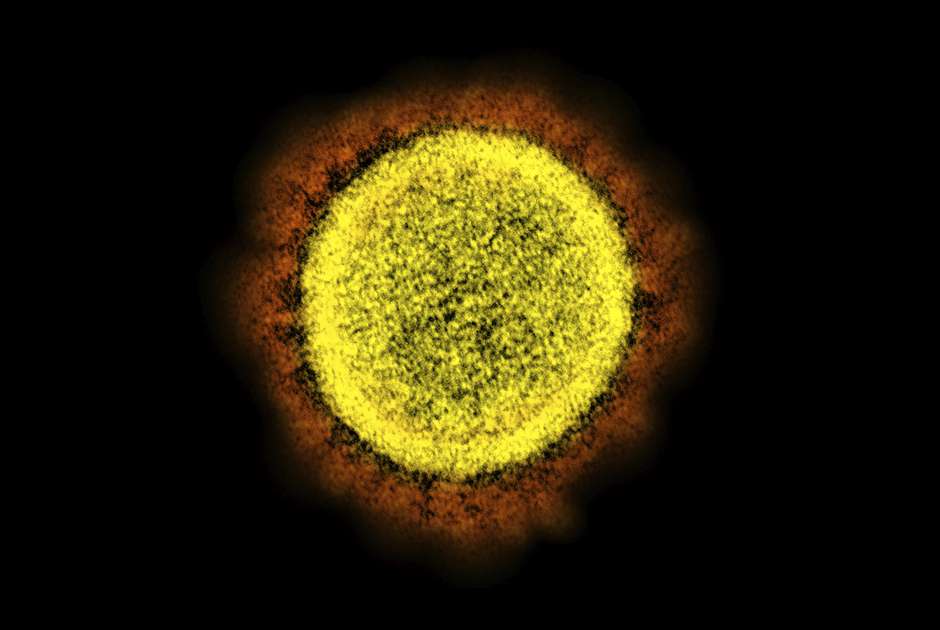
The researchers used data for about 1,100 counties between 1987 and 2017, so their results do not capture the effects of the coronavirus pandemic. However, crowded prisons have proven to be breeding grounds for COVID-19, and U.S. prisoners have so far been infected by the disease at a far higher rate than the general population.
The events of 2020 made reducing the number of people locked up in American jails more urgent than ever, Kajeepeta said, because her findings show that jails have contributed significantly to the spread of deadly infectious diseases like HIV and the flu in the broader population even before the coronavirus pandemic.
"Had we, at the start of the pandemic, massively reduced our jail populations, we likely would've avoided countless deaths," she said. "Jails and prisons have quickly become national epicenters for the virus."
The paper builds on another article published last year in the American Journal of Public Health by some of the same researchers in which they found that county jail incarceration rates were associated with overall county mortality rates. The purpose of this follow-up paper was to dig into the specific causes of death in order to give "more credence to the idea that we're picking up a causal effect rather than this being a spurious association," Kajeepeta said.
The most striking connections between inmate populations and overall mortality were picked up within a one-year time window. However, the researchers also examined the associations over five- and 10-year periods.
The associations decreased over longer periods of time, and the decrease was more pronounced for causes of death with shorter latency periods like suicide and overdoses, in comparison to longer-run diseases like cancer and diabetes.
Kajeepeta, who was formerly a leader at New York City Mayor's Office to End Domestic and Gender-Based Violence, said that she expects the worst effects of the association between incarceration and mortality would fall on racial minorities, even though the researchers were not able to break their findings down by race.
"We would expect these outcomes that we're seeing to fall along these racialized lines," she said, referencing a vast body of research showing that prisons disproportionately affect racial and ethnic minorities.
In addition to their quantitative findings, the researchers outlined three theoretical pathways through which incarceration may affect the health of the general public.
The first and most obvious pathway is the direct pathogenic effects of prison. Jails are often crowded and dirty, becoming petri dishes for diseases that spill over into the surrounding communities, the researchers said. Addicts who are incarcerated can also develop lower tolerances while in jail and therefore become more likely to overdose when they're released, according to Kajeepeta.
Another pathway is what the researchers called the "racialized psychosocial pathway," in which mass incarceration erodes trust in public institutions, as well as family and community ties.
"When we see this strong association with deaths due to suicide, this likely reflects this deprivation of psychosocial resources," said Kajeepeta.
And third, the researchers identified a potential economic link between jails and mortality. On the governmental level, spending on jails and prisons can come at the expense of public health and social welfare programs that reduce mortality from causes like diabetes and cancer, the researchers said. On a more individual level, incarceration removes workers from immediate employment, while criminal records can limit the job prospects of formerly incarcerated people for the rest of their lives.
"We know that jail incarceration disrupts local economies or labor markets by removing local people from the workforce," said Kajeepeta.
Kajeepeta said that while the three pathways were theoretical, she hopes that they serve as a useful framework for other researchers examining the health effects of incarceration.
Kajeepeta wrote the paper alongside her Columbia University Mailman School of Public Health Department of Epidemiology colleagues Pia Mauro, Katherine Keyes, Caroline Rutherford and Seth Prins, as well as Abdulrahman El-Sayed of Wayne State University in Detroit, Michigan.
Future studies with access to more extensive data should examine the connection between incarceration and overall mortality in relation to race, as well as the role of specific substances in increased overdose deaths, said Kajeepeta.
The paper, titled "Association between county jail incarceration and cause-specific county mortality in the USA, 1987–2017: a retrospective, longitudinal study," was published online in Lancet Public Health 2021. The authors are Sandhya Kajeepeta, Pia Mauro, Katherine Keyes, Caroline Rutherford and Seth Prins of the Columbia University Mailman School of Public Health Department of Epidemiology, as well as Abdulrahman El-Sayed of Wayne State University.
Correction: A previously published version of this article misidentified Sandhya Kajeepeta's former role at the New York City Mayor's Office to End Domestic and Gender-Based Violence. The error has been corrected.