Multiplying regulatory T cells could help treat inflammatory diseases
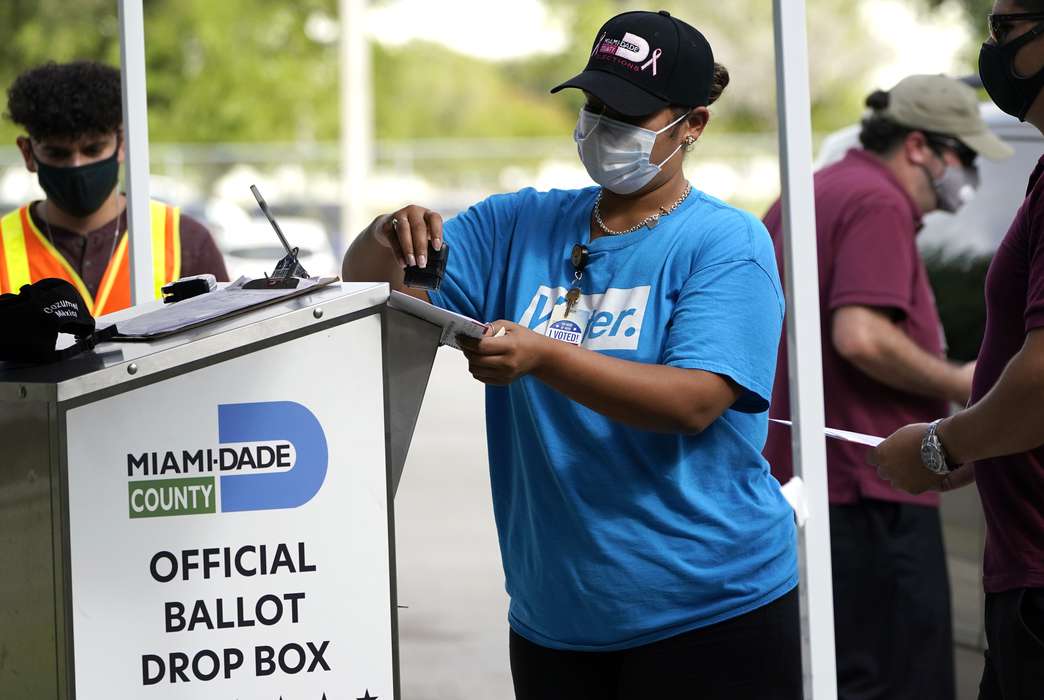
A human T cell under attack by a virus (in yellow). (AP Photo/Seth Pincus)
By adding a newly developed antibody to human cell cultures, researchers generated a greater number of more effective white blood cells that can slow a harmfully active immune system, according to a paper published in Science Signaling.
Using the antibody, the researchers caused rapid cell multiplication and boosted anti-inflammatory activity by activating a signaling receptor on regulatory T cells. The white blood cell variant discourages the immune system from attacking the body’s own tissues and causing autoimmune and other inflammatory diseases.
The receptor, tumor necrosis factor receptor 2 or TNFR2, also triggered a cascading effect in other receptors that led the cells to further proliferate.
The authors see the TNFR2 pathway as a promising low-risk alternative to standard treatments of inflammatory disorders — which suppress immune responses in a way that can leave patients vulnerable to infections and other side effects — as well as other pathways that make regulatory T cells multiply but are much more toxic.
Denise Faustman, the senior author of the paper, said TNFR2 is notable because it is excessively activated in cancer tumors but not activated often enough in people with autoimmune diseases.
“When you start seeing two major human disease pillars that abuse that receptor in opposite ways, you go, ‘That's a pretty interesting target,’” said Faustman, a researcher at Massachusetts General Hospital and an associate professor of medicine at Harvard University
The researchers developed and created the antibody in mice before adding it to cultures of human cells from healthy donors as well as those who had cancer or Type 1 diabetes, an autoimmune disorder. The regulatory T cells in all the samples grew in number and showed signs of increased potency in suppressing immune cells.
The TNFR2 pathway was demonstrated to be more effective than other methods of proliferating regulatory T cells, and previous research has shown that it is also less harmful. A 1996 study in baboons found TNFR2 can be activated without causing harmful side effects.
On the other hand, treating with the well-studied signaling protein Interleukin-2, or IL-2, is known to cause a wide range of side effects that include flu-like symptoms, low blood pressure and heart problems. Applying a form of signaling protein TNF to activate the receptor TNFR1 leads to an even longer list of harmful effects.
But these risky pathways are safely triggered as a downstream effect of activating TNFR2, Faustman said.
“It turns out when you tickle on a cell on TNFR2, it stimulates the IL-2 receptor that is a huge target,” she said, in addition to creating more TNF. “It's not just (that) you're increasing this receptor, but you're increasing these other receptors that are also important for regulatory T cell potency.”
In addition to possibly improving autoimmune diseases, increased numbers of regulatory T cells could reduce the chance of a transplanted organ being rejected, according to the researchers. The cell-multiplying treatment may also be used to treat neurodegenerative diseases or spinal cord conditions because of their healing effects in the central nervous system.
Before the agonist can be used as a treatment, Faustman said it needs to be first tested in monkeys and then in human clinical trials to identify possible side effects.
“Pending in vivo tests, these features indicate that this TNFR2 antibody agonist has the potential to safely and effectively treat various inflammatory disorders,” the researchers wrote.
The article, “A novel TNFR2 agonist antibody expands highly potent regulatory T cells,” was published Dec. 8 in Science Signaling.
The authors of the study were Heather Torrey, Willem Kühtreiber, Yoshiaki Okubo, Lisa Tran, Katherine Case, Hui Zheng, Eva Vanamee and Denise Faustman, Massachusetts General Hospital and Harvard Medical School. The lead authors were Heather Torrey and Willem Kühtreiber.